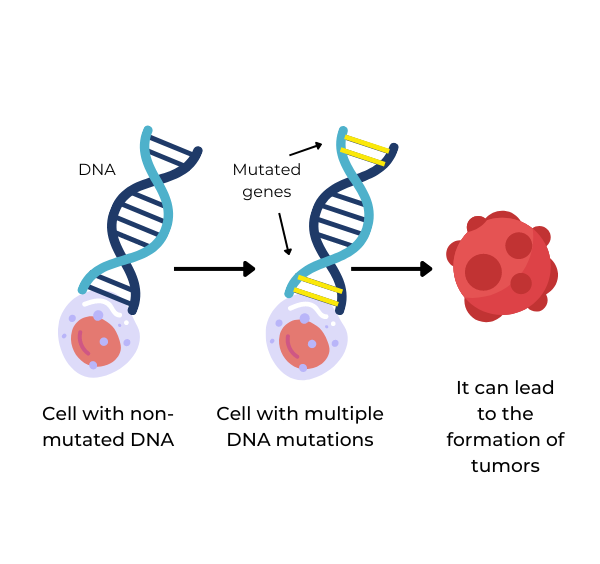
Cancer is a disease characterized by the uncontrolled proliferation of abnormal cells. At the heart of this disease lie mutations, which are changes in the genetic material of a cell that can result in unregulated cell growth. These mutations can occur in several forms and at various points within the human genome, affecting a diverse range of genes.
Understanding and treating these mutations is central to cancer research. Successful treatment strategies often hinge upon the identification and understanding of the specific gene mutations involved in the initiation and progression of cancer. This knowledge not only illuminates the biology behind cancer but also aids in the development of targeted therapies that can combat the disease.
Types of Cancer Mutations
Cancer-causing mutations can take multiple forms, each with different implications for cancer progression and treatment.
- Point Mutations: Changes in a single nucleotide, the smallest building blocks of DNA.
- Insertions and Deletions: The addition or removal of nucleotides from a DNA sequence. These changes can cause a frameshift in the genetic code, significantly altering the resulting protein and potentially leading to cancer.
- Chromosomal Translocations: The rearrangement of parts between nonhomologous chromosomes. This can lead to the formation of fusion genes that produce proteins with new functions, often leading to uncontrolled cell growth.
- Copy Number Alterations: Changes in the number of copies of a particular gene. These alterations can result in an excess or deficiency of the protein product, disrupting the delicate balance of cell growth and death.
Types of Mutated Genes in Cancer
Cancer is a complex disease that arises from a variety of genetic changes. These genetic mutations can be broadly categorized into two types: acquired mutations and germline mutations, each with distinct origins and implications for cancer development and treatment.
Acquired Mutations
Also known as somatic mutations, these are changes that occur in the DNA of individual cells during a person's lifetime. These mutations can result from exposure to various factors, including:
- Tobacco Use: Numerous harmful chemicals found in tobacco can damage DNA, leading to mutations. Notably, this is a significant factor in lung and oral cancers.
- UV Radiation: Overexposure to ultraviolet light from the sun or tanning beds can cause DNA damage, primarily leading to skin cancers.
- Viruses: Certain viruses, such as human papillomavirus (HPV) and hepatitis B and C, can integrate their genetic material into host cells, potentially causing harmful mutations.
- Aging: As individuals age, the chance of accruing DNA damage increases. This natural process can lead to the accumulation of mutations over time, increasing cancer risk.
Germline Mutations
Many mutations are inherited from a parent and are present in every cell of the body from birth. While these mutations constitute a small fraction of all cancers, they significantly increase the risk of developing certain types of cancer. Hence, identifying germline mutations can inform cancer prevention strategies and enable risk-reducing interventions.
Gene Variants Linked to Cancer
Certain gene variants, resulting from mutations, play critical roles in driving disease progression in cancer:
Tumor Suppressor Genes
Often likened to the brakes of a cell, these genes prevent uncontrolled cell growth and division. If mutated, they lose their normal function, leading to unchecked cell proliferation.
- BRCA1 and BRCA2 are two well-known examples of tumor suppressor genes. Mutations in these genes can lead to the development of breast and ovarian cancers.
- TP53 is another significant tumor suppressor gene. It regulates the cell cycle and prevents the formation of cancer.
Oncogenes
In contrast to suppressor genes, oncogenes can be thought of as the gas pedal of a cell, promoting cell growth and division. When mutated, these genes can be permanently activated, causing excessive cell growth and proliferation.
- The HER2 gene, when overexpressed or amplified, can promote aggressive growth in certain types of breast cancer.
- The RAS family of genes, including HRAS, KRAS, and NRAS, are often mutated in various types of cancer, including lung, colon, and pancreatic cancers.
DNA Repair Genes
These biological agents protect genomic integrity, repairing errors that occur during DNA replication. When repair genes themselves mutate, errors go unrepaired, leading to an accumulation of mutations and potentially cancer.
The Most Commonly Mutated Gene in Cancer
TP53, which produces a protein known as p53, is the most frequently mutated gene in human cancers. TP53 lies at the intersection of various signaling pathways that regulate cell growth and death, DNA repair, and genomic stability. Due to its central role in these processes, its inactivation can have severe consequences, leading to unchecked cell proliferation, a hallmark of cancer.
p53, the protein encoded by the TP53 gene, is often described as the ‘guardian of the genome.’ It is a transcription factor that controls the expression of numerous genes involved in cell cycle arrest, apoptosis (programmed cell death), senescence (cellular aging), DNA repair, and inhibition of angiogenesis (the formation of new blood vessels that tumors use to grow and spread). Thus, p53 plays a vital role in preventing the formation and progression of cancer.
Mutations in TP53 can lead to the production of a faulty p53 protein that is unable to regulate cell growth and death effectively, leading to uncontrolled cell division and, ultimately, cancer. Additionally, some TP53 mutations can result in a gain of function, where the mutant p53 protein acquires new, often detrimental abilities that can promote cancer development.
Research That Drives Cancer Treatment
A stronger understanding of the specific genetic changes that drive the development and progression of various cancers reveals potential targets for new treatments. By examining the mutation process, we can predict resistance patterns to current therapies and design drugs that have fewer side effects and are more personalized and effective.
LIDE delivers innovations in oncology translational research and immuno-oncology. Contact Global Vice President, Josh Caggiula today to learn more about our first-class research capabilities.